COPD – new version
Overview - COPD: Your Complete Guide to Understanding, Managing, and Living Better
Chronic Obstructive Pulmonary Disease (COPD) is a long-term lung condition that makes it hard to breathe. It affects millions of people around the world and is one of the leading causes of illness and death. COPD includes a group of diseases that block airflow and make it harder to get air in and out of the lungs. The good news? With the right care, people living with COPD can manage their symptoms and live full, active lives.
This guide is designed to help you learn everything you need to know about Chronic Obstructive Pulmonary Disease (COPD). Whether you’ve been recently diagnosed or are looking for better ways to manage your symptoms, you’ll find clear, up-to-date information on:
- What COPD is
- How it’s diagnosed
- What causes it
- Treatment options
- How to prevent flare-ups
- Tips for living well with COPD.
You’ll also find links to helpful tools, self-management programs, and educational resources to support your journey.
What is COPD?
COPD means Chronic Obstructive Pulmonary Disease. It is a chronic, progressive lung condition that makes it harder to breathe over time. COPD is an “umbrella” term for two major breathing diseases that cause airways to become obstructed or blocked: chronic bronchitis and emphysema. These diseases often occur together but can also appear separately. The condition develops slowly and worsens over time, but early diagnosis and treatment can greatly improve quality of life.
Doctors use a breathing test called spirometry to diagnose COPD. If your lung function remains below normal even after using a bronchodilator, it may confirm the presence of COPD.
Types of Chronic Obstructive Pulmonary Disease
COPD isn’t just one disease. It’s a mix of lung problems that look different for each person. The two most common conditions that fall under the COPD umbrella are emphysema and chronic bronchitis. People with COPD often have symptoms of both.
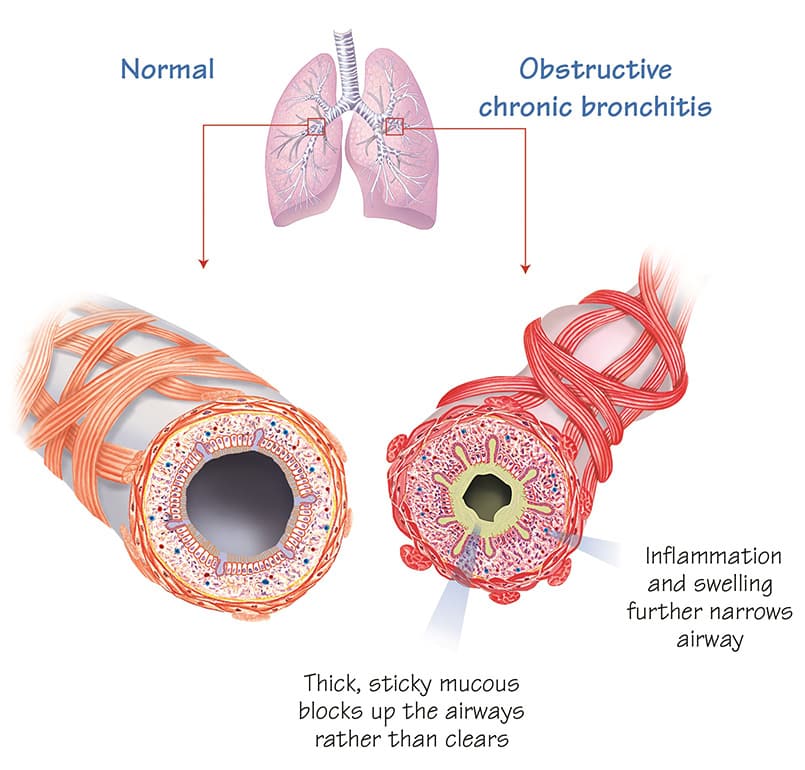
What is Obstructive Chronic Bronchitis?
When airways are constantly attacked by pollutants, such as cigarette smoke, they become inflamed and filled with thick, sticky mucus. You may cough to try to clear your airways. Over time, the bronchi (airways) may become obstructed or narrowed, meaning your lungs do not fully empty and air becomes trapped. This causes a persistent cough, frequent phlegm production, fatigue, and shortness of breath, especially during physical activities.
Symptoms and Causes of COPD
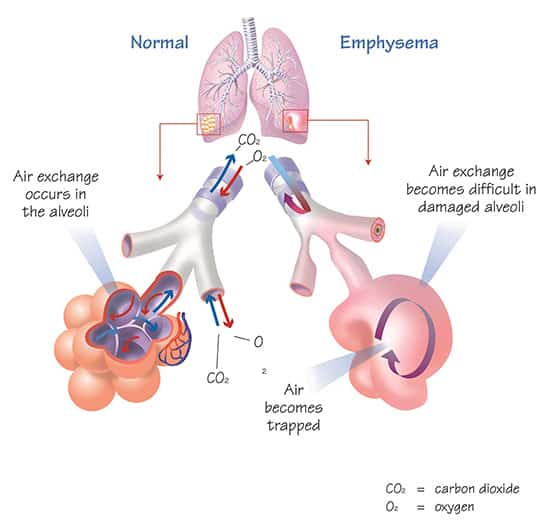
What is Emphysema?
Your bronchial tubes branch into smaller tubes that end in millions of tiny air sacs called alveoli. These sacs are where oxygen enters the blood and carbon dioxide is removed. In emphysema, the alveoli become damaged or destroyed, making it harder for the lungs to exchange gases. As a result, less oxygen reaches your body and your lungs do not empty fully. This trapped air causes breathlessness, especially during physical activity.
In emphysema, the tiny air sacs in the lungs (alveoli) become damaged or destroyed. These sacs are where oxygen enters the bloodstream and carbon dioxide is removed. When they’re damaged, the lungs struggle to exchange gases efficiently.
This causes:
- Less oxygen reaching the body
- Trapped air in the lungs
- Breathlessness during physical activity
Emphysema leads to reduced lung elasticity and makes it harder to exhale fully. It’s a major cause of breathlessness and fatigue in people with COPD. The damage is permanent, but with the right treatment plan, symptoms can be managed effectively.
Understanding the basics of COPD is the first step in learning how to manage it. In the next sections, we’ll talk about symptoms, diagnosis, treatment, and how to live better with COPD every day.
What Are the Symptoms of COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a condition that progresses over time and can affect people differently. However, some symptoms are especially common and may be present in early or more advanced stages. Recognizing them early can lead to better treatment outcomes.
Common symptoms of COPD include:
- Shortness of breath (dyspnea): This is the most common and troubling symptom for many patients. It often begins during physical activity and may get worse over time.
- Chronic cough: Often the first symptom to appear. It may start as occasional and become more frequent over time. It may or may not bring up mucus.
- Sputum (mucus) production: Many people with COPD cough up mucus, which may be thick and sticky. This is especially common in people with chronic bronchitis.
- Wheezing and chest tightness: Some people describe a whistling sound when they breathe, or a feeling of tightness in the chest, particularly after activity.
- Fatigue: Feeling tired, even without doing much, is common in COPD and can affect quality of life.
- Activity limitation: Over time, everyday activities like climbing stairs or walking can become more difficult.
- Exacerbations: These are sudden flare-ups of symptoms that may last for days or weeks. They often require extra treatment and may lead to hospital visits.
- Other signs in severe COPD: Weight loss, muscle wasting, ankle swelling, and depression or anxiety may appear in later stages of the disease.
When to See a Doctor
You should consult a healthcare provider if:
- You have ongoing breathlessness, a chronic cough, or frequent mucus production, especially if you have a history of smoking or exposure to harmful substances.
- Your symptoms suddenly get worse. This could indicate an exacerbation, which may require prompt treatment to avoid complications.
- You’re experiencing symptoms such as chest pain, high fever, or confusion.
- You have frequent lung infections or worsening fatigue.
Routine follow-ups are essential for monitoring your symptoms, treatment response, and potential complications.
What Causes COPD?
COPD is caused by a combination of factors that damage the lungs over time. It’s not caused by a single event but develops gradually, usually after years of exposure to harmful substances.
Main causes include:
- Cigarette smoking: This is the most common cause of COPD. Smoking damages the airways and lungs and speeds up lung aging. Even second-hand smoke can increase the risk.
- Air pollution: Indoor and outdoor air pollution, especially from burning wood or cooking fuels in poorly ventilated homes, can damage the lungs.
- Occupational exposures: Long-term exposure to dust, chemicals, or fumes in the workplace can increase COPD risk.
- Respiratory infections: Frequent lung infections, particularly in childhood, may impact lung development and increase future risk.
- Genetics: A rare inherited condition called Alpha-1 Antitrypsin Deficiency can lead to early-onset COPD, even in non-smokers.
- Other risk factors: Asthma, HIV, tuberculosis, low socioeconomic status, poor nutrition, and limited access to healthcare can contribute to disease development.
How Are the Lungs Affected?
COPD leads to long-lasting changes in the lungs:
- Airway damage: The small airways become inflamed, thickened, and narrowed. Mucus may block airflow, making breathing harder.
- Alveolar damage (emphysema): Tiny air sacs in the lungs (alveoli) become destroyed, making it harder to transfer oxygen into the blood.
- Lung hyperinflation: Because of blocked airflow, air gets trapped inside the lungs. This makes breathing difficult and reduces the ability to exhale fully.
- Gas exchange problems: Damaged lungs can’t properly exchange oxygen and carbon dioxide, leading to low oxygen levels in the blood.
- Chronic inflammation: Chronic exposure to irritants causes ongoing inflammation and cellular damage, even after quitting smoking.
These changes explain the common symptoms of COPD, shortness of breath, coughing, and fatigue, and why they get worse over time.
Cigarette Smoke and COPD
Cigarette smoke is the leading cause of COPD. Here’s how it affects the lungs:
- It damages lung tissue and causes inflammation.
- It increases mucus production and paralyzes tiny hairs (cilia) in the airways that usually help clear mucus.
- It accelerates lung function decline.
- Even low exposure (under 10 pack-years) and second-hand smoke can contribute to COPD.
- Smoking during pregnancy can affect lung development in the fetus.
Quitting smoking is the most effective step you can take to slow COPD progression and improve symptoms.
Nicotine replacement therapy and medications can support quitting. It’s never too late to stop smoking.
Thinking About Quitting Smoking? If you live with COPD, quitting smoking is one of the most powerful steps you can take to slow disease progression and breathe easier. Explore our free guide, “How to Quit Smoking,” filled with practical tips, support tools, and expert strategies to help you succeed, no matter where you are in your quit journey. 👉 Visit our Quit Smoking Guide
What Are the Risk Factors for COPD?
- Smoking: The number one risk factor. Long-term smokers are most at risk, but even occasional smoking can cause harm.
- Second-hand smoke exposure: Increases risk, especially with long-term exposure.
- Air pollution: Outdoor pollution and indoor smoke from cooking or heating fuels.
- Genetics: Alpha-1 Antitrypsin Deficiency and family history can increase susceptibility.
- Asthma and airway hyper-reactivity: Can lead to COPD or worsen symptoms.
- Infections: Childhood respiratory infections, HIV, and TB are associated with higher COPD risk.
- Socioeconomic status: Low income and poor access to healthcare are linked to worse outcomes.
- Occupational hazards: Prolonged exposure to dust, chemicals, or smoke in the workplace.
Understanding these risk factors can help you make informed choices about prevention and early detection.
Stay informed and talk to your healthcare provider if you have any concerns about your breathing or risk of COPD.
Complications of COPD: What You Should Know
Living with COPD doesn’t just affect your breathing, it can also lead to other health problems that impact your overall quality of life. Some of the most common complications include:
- Flare-ups (Exacerbations): Sudden worsening of symptoms like breathlessness, coughing, and mucus production. These episodes may require emergency care and can lead to faster disease progression.
- Heart Problems: People with COPD are at higher risk of conditions like high blood pressure, heart attacks, and heart failure, especially after a flare-up.
- Lung Infections: COPD makes you more vulnerable to infections like pneumonia or the flu, which can cause severe symptoms and hospitalization.
- Osteoporosis and Muscle Loss: Inactivity and inflammation can lead to weak bones and muscle wasting, increasing the risk of falls or fractures.
- Anxiety and Depression: Living with a chronic illness can affect your mental health. These conditions are common in people with COPD and can worsen physical symptoms if untreated.
- Sleep Disorders: COPD can affect sleep quality and may be linked to conditions like obstructive sleep apnea (OSA).
- Lung Cancer: COPD, especially when linked to smoking, increases your risk of developing lung cancer.
Managing COPD well and working with your healthcare team can help reduce the risk of complications. Treating the whole person, not just the lungs, is key to improving your health and quality of life.
What Are COPD Flare-Ups (Exacerbations)?
Flare-ups, or exacerbations, are sudden episodes when your COPD symptoms get worse than usual. You may feel more short of breath, have a stronger cough, or notice changes in your mucus, like more volume or a different color. These flare-ups can be triggered by infections (like colds or pneumonia), air pollution, or even weather changes.
Flare-ups are serious. They can lead to emergency visits, hospital stays, and long-term damage to your lungs. The more flare-ups you have, the faster your COPD may progress.
Managing COPD Flare-Ups (Exacerbations)
The good news is that many flare-ups can be prevented or managed early with the right tools and support. Here’s how:
- Know your symptoms. If your breathlessness, cough, or mucus suddenly get worse, act quickly.
- Follow your action plan. Work with your healthcare team to create a COPD Action Plan, a step-by-step guide for what to do when symptoms worsen.
- Use medications as prescribed. This includes rescue inhalers, corticosteroids, or antibiotics if your doctor recommends them.
- Avoid triggers. Stay away from smoke, pollution, or people with colds or the flu.
- Get vaccinated. Flu, COVID-19, and pneumonia vaccines can reduce your risk of flare-ups.
- Seek help early. Don’t wait until your symptoms are severe, call your healthcare provider as soon as something feels off.
Want to go deeper?
If you’re looking for practical tips on how to recognize, respond to, and recover from flare-ups, don’t miss our dedicated guide: How to Manage COPD Exacerbations.
It’s a helpful resource for building confidence, following your action plan, and reducing the impact of flare-ups on your daily life.
How Is COPD Diagnosed?
If you’ve been experiencing symptoms like frequent shortness of breath, a persistent cough, or mucus production, it’s time to talk to your doctor. These signs could point to Chronic Obstructive Pulmonary Disease (COPD), a condition that needs a proper diagnosis and plan.
The only way to confirm COPD is through a breathing test called spirometry. It measures how much air you can exhale and how quickly. If the test shows a post-bronchodilator FEV1/FVC ratio less than 0.7, it confirms airflow obstruction consistent with COPD.
What Happens During a Diagnosis?
Here’s what to expect when getting diagnosed:
- Medical history: Your healthcare provider will ask about your symptoms, smoking history, exposure to pollutants, and any history of lung infections.
- Spirometry test: This simple breathing test is quick, painless, and can be done in most clinics. It’s the gold standard for diagnosing COPD.
- Symptom assessment: Tools like the COPD Assessment Test (CAT) or mMRC Dyspnea Scale help evaluate how much your symptoms impact daily life.
- Exacerbation history: If you’ve had flare-ups (exacerbations) in the past year, especially those that required hospitalization, it helps determine the severity of your condition.
- Blood tests: as part of the evaluation your doctor will also run some blood tests.
- Comorbidities check: Other health issues (like heart disease, osteoporosis, or anxiety) are common in COPD and should be discussed as part of your care plan.
What Tests Are Used to Evaluate COPD?
Beyond spirometry, other tests may be used to get a clearer picture of how COPD is affecting your lungs and overall health:
- Pulmonary function tests: These measure how much air your lungs can hold and how much is trapped. Not always needed but helpful in some cases.
- Pulse oximetry: A small device placed on your finger to see how much oxygen is in your blood.
- Arterial blood gases (ABG): A more detailed blood test done if your oxygen levels are low or if you’re showing signs of respiratory failure.
- Chest X-ray: Not used to diagnose COPD, but helpful to rule out other conditions like heart problems or lung infections.
- CT scan: Provides a detailed look at lung damage, especially in cases of emphysema or repeated flare-ups.
- Genetic testing: If you’re under 45 or never smoked but have COPD, your doctor might test for alpha-1 antitrypsin deficiency, a rare inherited form of the disease.
COPD Treatment and Management
Managing Chronic Obstructive Pulmonary Disease (COPD) is not one-size-fits-all. Every person is different, so treatment is tailored to your specific symptoms, risks, and needs. The main goals are to help you breathe better, stay active, reduce flare-ups (exacerbations), and improve your quality of life.
Medical Treatments (Medications)
Most people with COPD use daily inhalers to help open their airways and reduce inflammation.
- Bronchodilators: These are medications that relax your airway muscles and make breathing easier.
- Short-acting bronchodilators are used as needed.
- Long-acting bronchodilators (like LAMA or LABA) are used every day to keep your lungs open.
- Inhaled corticosteroids (ICS): These reduce inflammation and help prevent flare-ups. They are often combined with bronchodilators in one inhaler.
- Triple Therapy (LAMA + LABA + ICS): For people with more severe symptoms or frequent flare-ups, a single inhaler with all three medications may be recommended.
- Other medications: In some cases, your doctor may add antibiotics (for infections), mucolytics (to loosen mucus), or other pills like roflumilast if symptoms persist.
👉 Always use your inhaler exactly as instructed, and ask your healthcare provider to check your technique regularly.
Non-Medical Treatments (Lifestyle & Support)
Medications are important, but they’re not the whole story. These lifestyle changes and support strategies also make a big difference:
- Quit Smoking: The most important step. Stopping smoking slows disease progression and improves symptoms.
- Vaccines: Stay protected against flu, pneumonia, COVID-19, and other infections.
- Pulmonary Rehabilitation: This is a program that combines exercise, education, and breathing techniques. It helps you stay active and improve your stamina.
- Healthy Habits: Eating well, staying physically active, and managing stress support overall lung health.
- Oxygen Therapy: If your oxygen levels are low, you may benefit from supplemental oxygen, especially during sleep or activity.
- Supportive Care: For advanced COPD, palliative care and counseling can help you manage symptoms like breathlessness and anxiety.
Regular Checkups Matter
Managing COPD is an ongoing process. Make sure to:
- Have your lung function tested regularly (spirometry).
- Review your inhaler technique and medications.
- Report any new symptoms or flare-ups.
- Talk to your care team about vaccinations and lifestyle support.
Prevention of COPD
Chronic Obstructive Pulmonary Disease (COPD) is a serious and progressive lung condition, but the good news is that it’s largely preventable. Whether you’re looking to avoid COPD or trying to slow its progression after being diagnosed, there are effective steps you can take to protect your lungs and improve your quality of life.
Can COPD Be Prevented?
Yes, in many cases, COPD is preventable. The number one way to lower your risk is to avoid or quit smoking. Smoking damages the lungs and is the leading cause of COPD worldwide. If you smoke, quitting is the most important step you can take for your lungs. Even after years of smoking, quitting can slow the disease and help you breathe easier.
Other important prevention tips include:
- Avoid secondhand smoke and polluted environments.
- Use protective equipment if you work around dust, fumes, or chemicals.
- Cook with proper ventilation if you use wood or biomass fuel at home.
- Get vaccinated. Infections like flu and pneumonia can trigger COPD or make it worse.
- Get regular checkups, especially if you’ve had frequent chest infections or breathing issues.
How to Prevent COPD from Getting Worse
If you’ve already been diagnosed with COPD, preventing flare-ups and slowing disease progression is key. Here’s how:
Medical Treatment
- Use your inhalers or medications exactly as prescribed.
- Ask your doctor to review your medications if your symptoms are not properly controlled, or side effects are bothering you.
- If you’ve had multiple flare-ups, additional medications may be needed to keep your lungs stable.
Vaccinations
- Stay up to date on flu, COVID-19, RSV, and pneumonia vaccines to reduce your risk of serious infections.
Lifestyle Support
- Ask your doctor to refer you to a pulmonary rehabilitation program to improve your strength, breathing, and confidence.
- Eat well, stay active, and get enough rest.
- Monitor your symptoms and act early if you feel a flare-up coming on.
Self-Management and Education
- Work with your healthcare team to create an action plan to prevent flare-ups, recognize them early and take rapid action when they occur.
- Learn breathing techniques and proper inhaler use.
- Ask questions. Understanding your condition helps you take control of it.
Living Well with COPD
Living well with COPD is possible, and it starts with the right plan, the right tools, and the right support.
Chronic Obstructive Pulmonary Disease (COPD) can affect many parts of your life, but with the right approach, you can breathe easier, stay active, and feel more in control of your health. Whether you’ve just been diagnosed or have lived with COPD for years, this section will help you understand how to manage your symptoms and improve your day-to-day life.
Key Elements of a Healthy COPD Lifestyle
To truly live well with COPD, your care plan should include both medical treatments and daily habits that support your lungs and overall health.
Here’s what works:
- Use Your Medications Correctly: take your medications every day as prescribed. Your medications can help you breathe better and prevent flare-ups. Use your inhaler correctly. Ask your healthcare provider to show you the right technique.
- Stay Active With Confidence: Stay physically active, even with light movement like walking or stretching. It strengthens your lungs and boosts your mood.
- Learn to Manage Flare-Ups: At the first sign of worsening symptoms, act quickly. Use your COPD Action Plan to know what steps to take and when to call your doctor.
- Breathe Easier at Home: If your oxygen levels are low, your doctor may prescribe oxygen therapy or a home breathing device to help you rest and recover.
- Take Care of Your Mind, Too: Take care of your mental health. Anxiety and depression are common but treatable with support and breathing techniques.
- Stay on Track With Routine Care: Keep up with regular check-ups, stay vaccinated (flu, pneumonia, RSV, COVID-19), track your progress with tools like the COPD Assessment Test (CAT), and manage other conditions like heart disease or diabetes.
New: Updated COPD Learning Modules – April 2025
To help you live better with COPD, we’ve just released the updated Living Well with COPD™ Modules — now available online and free of charge.
These interactive, patient-focused lessons cover topics like:
- Managing stress and anxiety
- Staying active with exercise
- Using oxygen therapy at home
- Understanding your medications
- Avoiding triggers and preventing flare-ups
Create your account for free and join thousands of patients already using our expert-backed tools to take control of their condition.
A Note from RESPIPLUS
At RESPIPLUS, our mission is to empower patients and healthcare professionals with trusted, evidence-based tools to manage chronic respiratory diseases like COPD. We believe that with the right support, education, and care, people with COPD can live active, fulfilling lives.
This page is part of our commitment to sharing up-to-date, accessible resources, like the new 2025 edition of the Living Well with COPD™ modules, now available for free. These interactive guides are designed to help you take control of your health, understand your condition, and feel more confident every day.
👉 Create a free account today to explore over 10 modules designed by experts and patients alike: www.chroniclungdiseases.com/register
FAQ About COPD
What is COPD and how does it affect the lungs?
COPD stands for Chronic Obstructive Pulmonary Disease. It includes conditions like chronic bronchitis and emphysema that make it hard to breathe by damaging the airways and air sacs in the lungs. Over time, this damage causes airflow limitation that can’t be fully reversed.
What is the main cause of COPD?
The most common cause is long-term exposure to harmful substances like cigarette smoke. Other causes include air pollution, workplace fumes, and certain genetic conditions like Alpha-1 antitrypsin deficiency.
Is COPD the same as asthma?
No. While both affect breathing, COPD is usually progressive and linked to long-term exposure to irritants, while asthma is often related to allergies and can be reversible with treatment.
What’s the difference between emphysema and chronic bronchitis?
Emphysema damages the tiny air sacs in your lungs (alveoli), reducing your lungs’ ability to exchange oxygen. Chronic bronchitis involves inflammation in your airways and leads to persistent cough with mucus. Many people with COPD have features of both.
Is COPD contagious?
No. COPD isn’t contagious. You can’t catch it from someone else. COPD develops over time due to lung damage from things like smoking or breathing in harmful particles.
What are the first signs of COPD?
Early symptoms include shortness of breath (especially during physical activity), a lingering cough, and excess mucus production. If you notice these signs, particularly if you smoke or used to smoke, it’s important to talk to your doctor.
How do I know if I have COPD?
If you experience persistent cough, shortness of breath, or frequent chest infections, ask your doctor about COPD. A simple breathing test called spirometry can confirm the diagnosis by measuring how well your lungs work.
What stage of COPD am I in?
COPD is classified into stages based on how much airflow is blocked, using a test called spirometry. Your doctor can explain what stage you’re in and how it affects your treatment plan.
Can COPD be cured?
There is no cure for COPD, but it can be treated. With medications, healthy habits, and the right care plan, many people live well and manage their symptoms.
Can a person with COPD get better?
Yes, while COPD can’t be cured, symptoms often improve with treatment, lifestyle changes, and pulmonary rehab. Many people find they can breathe better, feel stronger, and do more over time.
Can you live a long life with COPD?
Yes. With early diagnosis and consistent treatment, many people with COPD live for years, even decades. Quitting smoking, exercising, and using medications properly can make a big difference.
Can I live a normal life with COPD?
Absolutely. With the right care and adjustments, people with COPD can stay active, enjoy hobbies, travel, and maintain a fulfilling lifestyle.
Is COPD a terminal illness?
COPD is a serious, long-term disease, but it’s not always terminal. Many people live for a long time when it’s managed well. Some cases become severe, but early care and support improve outcomes.
What treatments are available for COPD?
Treatment may include inhalers (like bronchodilators and corticosteroids), pulmonary rehabilitation, vaccines, oxygen therapy (if needed), and lifestyle changes such as quitting smoking and staying active.
Do I need to be on oxygen if I have COPD?
Not always. Oxygen therapy is used if your blood oxygen levels are low. Your doctor will check your oxygen with a simple test and let you know if it’s needed.
Should I still exercise with COPD?
Yes. In fact, exercise can improve your breathing, energy, and mood. Even gentle activities like walking or stretching can make a difference. Pulmonary rehab programs are especially helpful.
What triggers a COPD flare-up (exacerbation)?
Flare-ups can be caused by infections, cold air, air pollution, smoke exposure, or missing medications. Symptoms like worse breathing, more coughing, or thicker mucus may signal a flare-up.
What should I do during a COPD flare-up?
Follow your COPD Action Plan, take your rescue medications as prescribed, and contact your healthcare provider if symptoms don’t improve. Acting quickly can help prevent complications or hospital visits.
Related Articles
If you want to keep learning about COPD and related topics, check out these articles:
COPD - Resources for patients
Please note these links will bring you to the respective organizations’ websites, these educational materials are not handled by RESPIPLUS.
Specific Resources | COPD
- Living Well With COPD
- COPD Canada
- You Can Make it Happen
- Alpha-1 Canada
- AlphaNet Canada
- Alpha-1 Canadian Registry
- COPD Action Plan
General Resources | Lung diseases
- Canadian Lung Association (CLA)
- Alberta & NWT Lung Association
- British Columbia Lung Association
- Manitoba Lung Association
- New Brunswick Lung Association
- Newfoundland & Labrador Lung Association
- Nova Scotia Lung Association
- Lung Health Foundation (previously the Ontario Lung Association)
- Prince Edward Island Lung Association
- Quebec Lung Association (QLA)
- The Lung Association, Saskatchewan (LAS)
COPD - Resources for health professionals
Please note these links will bring you to the respective organizations’ websites, these educational materials are not handled by RESPIPLUS.
Guidelines | COPD
CLINICAL PRACTICE GUIDELINE FOR THE PHARMACOTHERAPY OF COPD The Canadian Thoracic Society (2023)
- GLOBAL STRATEGY FOR PREVENTION, DIAGNOSIS AND MANAGEMENT OF COPD: 2025 Report
Specific Resources | COPD
- Living Well With COPD
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)
- Understanding COPD Questionnaire (UCOPD)
- CDM Quality Care in COPD
General Resources | Lung diseases
- Canadian Thoracic Society (CTS)
- Canadian Lung Association (CLA)
- RESPTREC – Respiratory Training & Educator Course
- Réseau québécois d’éducation en santé respiratoire (RQESR) (French only*)
- REHABforhealth
- Help Them Quit
- iMD – Library of visual medical content
- American Thoracic Society (ATS)
- European Respiratory Society (ERS)

