PULMONARY FIBROSIS - General Information
What is Pulmonary Fibrosis?
Pulmonary Fibrosis (PF), also known as interstitial lung disease, is a disease that can affect every part of your life. As the disease progresses, so will its impact on your daily activities. The exacerbations of the disease, or periods of worsening symptoms, can greatly affect your quality of life.
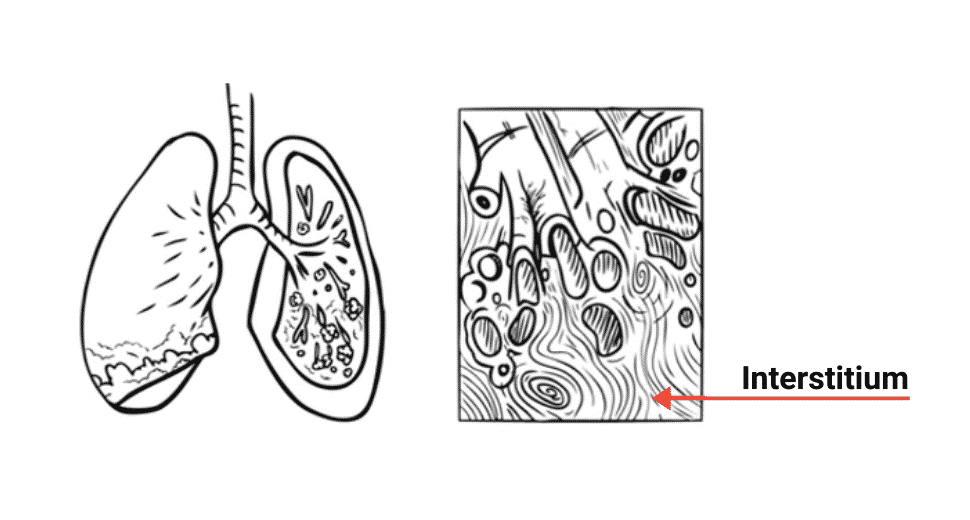
Pulmonary fibrosis is a disease characterized by progressive scarring in the lungs. This scar formation causes the lung interstitium (the part of the lung where gas exchange occurs) to become thicker and stiffer. When you breathe in, oxygen needs to diffuse through the interstitium to reach the blood circulation. In pulmonary fibrosis, the thickened interstitium makes it harder for oxygen to reach the blood, leading to breathlessness and other symptoms.
What is Idiopathic Pulmonary Fibrosis (IPF)?
While many types of pulmonary fibrosis are linked to a specific cause, Idiopathic Pulmonary Fibrosis (IPF) is the most common form. The term “idiopathic” means the exact cause is unknown. IPF is a chronic and progressive disease that, without effective management, can lead to severe complications. Given its prevalence, it is a primary focus of research and patient care.
Table of Contents
Healthy vs Fibrotic Lung
Healthy Lung

Fibrotic Lung
Symptoms and Causes of Pulmonary Fibrosis (PF)
What are the symptoms of Pulmonary Fibrosis?
The diagnosis of pulmonary fibrosis can be challenging because its initial symptoms often mimic those of more common conditions. Be aware of the following signs:
- A gradual onset of shortness of breath, especially during physical activity.
- A persistent, dry, hacking cough that does not produce mucus.
- Fatigue and general weakness.
- Unexplained weight loss.
- Aching muscles and joints.
- Clubbing (the widening and rounding of the tips of the fingers or toes).
When to see a doctor
If you are experiencing these symptoms, or if your symptoms are worsening, it is crucial to consult a healthcare professional. Early and accurate diagnosis is essential for effective management and improved outcomes.
What causes Pulmonary Fibrosis?
While the exact cause of IPF remains unknown, several factors and conditions are known to be linked to other types of pulmonary fibrosis:
- Environmental Exposure: Long-term exposure to hazardous materials such as asbestos, silica dust, or bird and animal droppings.
- Medical Conditions: Certain autoimmune diseases (like rheumatoid arthritis or lupus) and chronic acid reflux.
- Medications: Some drugs used to treat heart conditions, chemotherapy, or certain antibiotics.
- Genetics: In some cases, pulmonary fibrosis runs in families.
What are the risk factors of PF?
- Smoking: A significant risk factor for many types of lung disease, including pulmonary fibrosis.
- Age: The disease is more likely to affect middle-aged and older adults.
- Gender: Idiopathic pulmonary fibrosis is more common in men.
- Family history: A genetic predisposition can increase your risk.
Diagnosis and Tests
How is Pulmonary Fibrosis diagnosed?
Diagnosing pulmonary fibrosis and identifying the precise type of fibrosis is a challenging process. This disease may be difficult to diagnose and you may need to see many doctors before knowing what type of pulmonary fibrosis you have. Many tests including pulmonary function tests, medical imagery and blood tests may be necessary to determine the type of pulmonary fibrosis you have.
Learn more about this topic by downloading your free personal copy of “Dealing with a diagnosis of Pulmonary Fibrosis” of the Living Well with Pulmonary Fibrosis program.
To access the full program, create a free account on ChronicLungDiseases.com. Once logged in, you can explore all modules at your own pace and access a wide range of resources, including information brochures, learning materials, videos, and more.
What tests do healthcare providers use to diagnose PF?
Many tests are necessary to determine the type and extent of your pulmonary fibrosis, including:
- Pulmonary Function Tests (PFTs): These tests measure how well your lungs are working, including your lung size and air flow.
- High-Resolution Computed Tomography (HRCT) Scan: The most important imaging test. It provides detailed images of your lungs to look for the characteristic scarring patterns of pulmonary fibrosis.
- Blood Tests: Used to rule out other diseases and identify conditions that may be linked to the fibrosis.
- Surgical Lung Biopsy: In some cases, a small piece of lung tissue is removed and examined to confirm a diagnosis and determine the specific type of fibrosis.
Diagnosing pulmonary fibrosis and identifying the precise type of fibrosis is a challenging process
Management and Treatment of Pulmonary Fibrosis
How is Pulmonary Fibrosis managed?
The treatment of pulmonary fibrosis takes many forms and may change throughout the course of your disease. It is important to follow all treatment plans as prescribed by your physician. A comprehensive treatment plan includes:
- Medication: Anti-fibrotic medications and, in some cases, immunosuppressive drugs. These medications do not cure pulmonary fibrosis, but they may help reduce the progression of the disease.
- Flare-up Management: Preventing and controlling sudden worsening of symptoms (exacerbations) and having a plan to treat them when they occur.
- Oxygen Therapy: Recommended for some individuals to help manage shortness of breath.
- Pulmonary Rehabilitation: A structured program to engage in physical activity and exercise with the support of a healthcare team.
- Lifestyle Changes: Making lifestyle adjustments to stay as healthy as possible.
- Lung Transplant: For certain eligible individuals, a lung transplant may be a treatment option.
What is a multidisciplinary approach to care?
Effective management of pulmonary fibrosis requires a multidisciplinary approach. You will work with a team of specialists, including a pulmonologist, a respiratory therapist, a nutritionist, and a social worker or counselor, to ensure all aspects of your health are addressed.
Living Well with Pulmonary Fibrosis (PF)
Can people with Pulmonary Fibrosis get better?
A diagnosis of pulmonary fibrosis can change the way you see yourself. You may feel trapped, isolated, of no use to your family and friends. You may feel hopeless. These are common reactions.
But remember, you are not alone and there are many ways in which you can learn about how to regain control of your life with pulmonary fibrosis. You can discuss your concerns with your doctor or resource person. Patient support groups are a very helpful resource for gaining understanding of how to deal with the disease.
Practical tips for improving quality of life
- Stay Active: Engage in regular physical activity. A pulmonary rehabilitation program can provide tailored exercises to help you breathe easier and improve your stamina.
- Eat Healthy: Maintaining an ideal weight and following a balanced diet can reduce the strain on your lungs and improve your energy levels.
- Stay Informed: The more you know about your condition, the more empowered you will feel. Work together with your healthcare team to get information specifically suited to your needs.
The Living Well with Pulmonary Fibrosis program offers information and support for each of these topics. The best way to learn more about Pulmonary Fibrosis is to work together with your healthcare team that will be able to provide you with the information and support specifically suited to your needs.
The program consists of the following modules:
- Dealing with a Diagnosis of Pulmonary Fibrosis
- Adopting & Maintaining a Healthy & Fulfilling Lifestyle
- Treating Pulmonary Fibrosis
- Managing the Impact of Pulmonary Fibrosis
- An Action Plan for When Your Symptoms Get Worse
- Get Moving…Breathe Easy with Pulmonary Fibrosis
- Integrating Long-Term Oxygen Therapy Into Your Life
- Pulmonary Fibrosis & End of Life
To access the full program, create a free account on ChronicLungDiseases.com. Once logged in, you can explore all modules at your own pace and access a wide range of resources, including information brochures, learning materials, videos, and more. Healthcare professionals also have access to tools specifically designed to support patient education.
you are not alone & there are many ways in which you can learn about how to regain control of your life with pulmonary fibrosis.
A Note from Respiplus
At Respiplus, we understand that living with pulmonary fibrosis can be challenging, but we want you to know that you are not alone on this journey. Our mission is to provide you with the knowledge and tools you need to take an active role in your care. This educational program was created with you in mind, to empower you to feel more in control of your life with PF. We are here to help you live well.

Frequently Asked Questions (FAQ) about Pulmonary Fibrosis
What is the difference between Pulmonary Fibrosis (PF) and Idiopathic Pulmonary Fibrosis (IPF)?
"Pulmonary Fibrosis" is a general term for scarring of the lungs from various causes. Idiopathic Pulmonary Fibrosis (IPF) is a specific type of pulmonary fibrosis where the exact cause is unknown. IPF is also the most common and severe form of the disease and has specific FDA-approved treatments that may not be used for other types of PF.
Is Pulmonary Fibrosis contagious or hereditary?
Pulmonary fibrosis is not contagious. You cannot catch it from another person. While PF can run in families in some cases (familial pulmonary fibrosis), it is not a hereditary disease for everyone. It is important to inform your doctor if there is a family history of the disease.
What are the stages of pulmonary fibrosis?
PF is typically a progressive disease, but it does not follow a strict, linear staging system like some cancers. Instead, doctors assess the severity of the disease based on how it impacts your lung function, symptoms, and quality of life. The progression varies greatly from person to person.
At what age does pulmonary fibrosis start?
Pulmonary fibrosis can occur at any age, but it is most commonly diagnosed in adults over the age of 50. The risk increases with age.
What is the role of a caregiver in managing Pulmonary Fibrosis?
A caregiver's role is vital. It includes providing emotional support, helping to manage medications and appointments, and assisting with daily activities. Caregivers also play a key part in monitoring symptoms and communicating with the healthcare team.
What are the first signs of Pulmonary Fibrosis?
The first signs of pulmonary fibrosis are often subtle and can mimic other diseases. They include a persistent dry cough, shortness of breath, fatigue, and a feeling of being unwell. These symptoms often get worse over time.
How is Pulmonary Fibrosis diagnosed?
Diagnosis is a multi-step process that requires a healthcare provider to combine information from your medical history, a physical exam, and specialized tests. The most important tests for diagnosis are the High-Resolution CT (HRCT) scan and Pulmonary Function Tests (PFTs).
How is Pulmonary Fibrosis different from COPD or asthma?
The key difference lies in the nature of the disease. PF involves the scarring and stiffening of lung tissue, making it harder for oxygen to enter the bloodstream. COPD and asthma are typically characterized by airway obstruction (airflow blockage) and inflammation, making it difficult to breathe air out.
Can Pulmonary Fibrosis be cured?
Currently, there is no cure for pulmonary fibrosis. However, there are a variety of treatments and therapies that can help slow the progression of the disease, manage symptoms, and improve a person's quality of life.
How is Pulmonary Fibrosis treated?
Treatment involves a comprehensive plan that may include anti-fibrotic medications, oxygen therapy to manage breathing difficulties, and pulmonary rehabilitation to improve physical function. For some eligible patients, a lung transplant may be an option.
What triggers a Pulmonary Fibrosis flare-up (exacerbation)?
A flare-up, or exacerbation, is a sudden and significant worsening of symptoms. This can be triggered by infections like the flu or pneumonia, or sometimes the cause is unknown. It's crucial to contact your doctor immediately if you notice a sudden change in your symptoms.
Can you live a long life with PF?
While pulmonary fibrosis is a serious disease that can shorten life expectancy, it's important to remember that each person's experience is unique. With proper management, including medications, rehabilitation, and lifestyle changes, many people with PF can live for many years and maintain a good quality of life.
Do I need to be on oxygen if I have Pulmonary Fibrosis?
Not everyone with pulmonary fibrosis will need oxygen therapy. A doctor will determine if it is right for you, based on your oxygen saturation levels. Using oxygen will not make your condition worse, and it can help you feel better and do more.
Should I still exercise with Pulmonary Fibrosis?
Yes. Regular physical activity, as prescribed by your doctor or a pulmonary rehabilitation program, is highly recommended. Exercise can help strengthen your heart, lungs, and muscles, making you feel less short of breath and significantly improving your ability to perform daily activities.
Can I travel with Pulmonary Fibrosis?
Yes, many people with pulmonary fibrosis travel. It's important to consult with your doctor before any trip, especially if you plan to fly, as you may need to arrange for oxygen during the flight. Planning ahead is key to a safe and enjoyable trip.

